Can we use artificial intelligence (AI) to better diagnose fractures?
Dr Susan Shelmerdine, Consultant Paediatric Radiologist at Great Ormond Street Hospital (GOSH), has received almost £1 million in funding as part of a NIHR Advanced Fellowship for her research into using artificial intelligence (AI) to identify fractures in children.
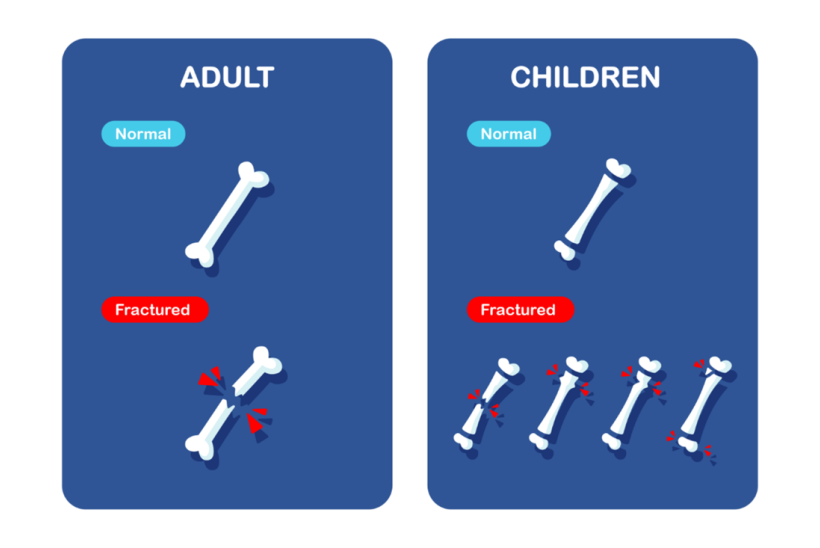
Half of all children will sustain a fracture (broken bone) at some point in their childhood. Almost all of these will require an X-ray to diagnose and help guide further treatment, but these injuries can be hard to spot. This is particularly the case in children, where growing bones can look like fractures on X-ray images and subtle fractures (common in many children) can appear different to those seen in adults.
Accurate detection of fractures often requires the specialist knowledge of paediatric radiologists, yet many hospitals across the country do not have regular access to this expertise. This can lead to missed diagnoses which in turn prolongs pain and discomfort for the children involved and repeated visits to the hospital and days missed from school.
Dr Susan Shelmerdine’s new 5-year research project aims to develop a computer programme (using artificial intelligence) that will help emergency doctors and nurses across the country to better identify fractures in children.
Bringing expertise to the masses
Through a collaboration with different trauma hospitals across the UK, Dr Shelmerdine is building a large database of X-ray images of children’s bones. This bank of images will be used to train a computer programme to spot bones with fractures. The aim is for the programme to identify factures with a similar accuracy to specially trained paediatric radiologists.
Dr Shelmerdine will then take the programme to emergency doctors and nurses who do not regularly have access to the expertise of paediatric radiologists and check to see how the results of the computer programme may affect their decision making and diagnostic accuracy. The purpose of this technology is to assist healthcare staff in their diagnosis, not to replace their role.
Paediatric radiologists have expert knowledge to spot fractures in children quickly and accurately, but not all hospitals will have these sorts of specialists. I’m hoping that my research will bring that expertise to every hospital in the country, meaning all children will have access to the best care.
Dr Susan Shelmerdine, Consultant Paediatric Radiologist

Involving patients every step of the way
Dr Shelmerdine is acutely aware that bringing in new methods of diagnosis should not be done without incorporating the opinions of the children and families that the new tools will directly impact.
She has been working closely with members of the GOSH Young Persons Advisory Group (YPAG) and the GOSH Parent and Carer Advisory Group throughout this study to ensure that patient views are always heard. Seven young persons and carer members have volunteered to form a ‘FRACTURE study’ steering group for this study and provide guidance and views on how the work is being conducted.
They have worked collaboratively to design a national public survey, forming the central focus of Dr Shelmerdine’s first year of research. This survey is aiming to understand how children and their caregivers feel about using artificial intelligence (AI) as part of their diagnosis and the best way to introduce it as part of routine care.
If you are a young person or have caring responsibilities for children and young people, you can also take part in this research.
During the later phases of the study, Dr Shelmerdine will engage YPAG members to help create engaging content and explain AI to children and staff who will be using the computer programme in the future.
You can find out updates and get involved on the FRACTURE study site.