Innovative Solutions for ROHHAD: Salem's transformation through Phrenic Nerve Pacing at GOSH
Salem is a young boy from Qatar, who was diagnosed with ROHHAD (Rapid-onset Obesity, Hypothalamic dysfunction, Hypoventilation, and Autonomic Dysregulation) at the age of 4 years.
ROHHAD is a rare condition in children where they quickly gain weight during the first two to four years of life, often accompanied by endocrine disorders, hypoventilation (shallow breathing), and autonomic dysregulation (problems with the autonomic nervous system that controls involuntary bodily functions). Salem’s main medical issue was hypoventilation, which reduces his ability to take in sufficient oxygen and exhale carbon dioxide from his body. This required him to have mechanical ventilation, where a breathing machine was used to pump air in and out of his lungs via a face mask at night during sleep. Salem’s breathing problem worsened so that ventilation at night alone was insufficient, and he ended up needing ventilatory support attached to a face mask most of the day too.
Salem's family sought advice from a North American hospital, who confirmed that Salem had severe hypoventilation and needed mechanical ventilation for 24 hours per day. The 24-hour requirement meant that mask ventilation would not be sustainable long term. Instead, the American doctors advised a tracheostomy, an operation involving the permanent placement of a tube in his airway through the front of the neck.
Salem’s family were not keen on this option, as Salem was otherwise in good health. However, upon learning Great Ormond Street Hospital (GOSH) 's skills in providing care for children with complex conditions, and with the recommendation of Dr Paul Aurora by a Qatari consultant, Salem's family decided to transfer from the USA to GOSH for a second opinion.
Before coming to GOSH, we searched for Dr Paul Aurora and learned that he specialises in rare cases like Salem's. Dr Aurora was a glimmer of hope for us.
Salem’s Grandmother

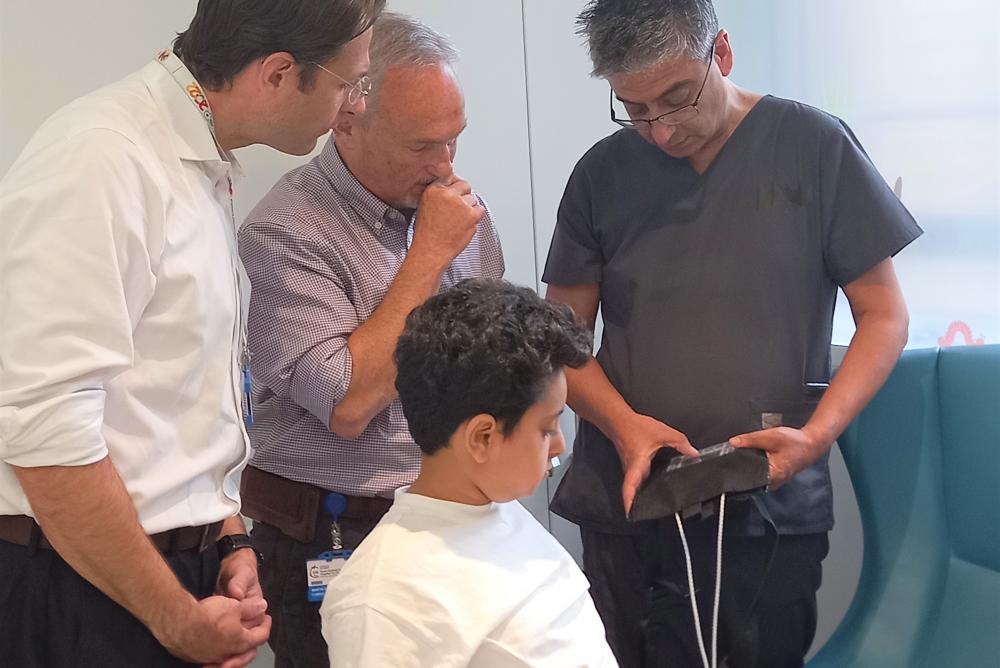
Upon arriving at GOSH, Salem underwent a comprehensive evaluation by Dr Paul Aurora and a team of doctors, including experts in sleep medicine and long-term ventilation in children, Dr Martin Samuels and Dr Elaine Chan. The team confirmed that Salem was experiencing severe hypoventilation, requiring a minimum of 20 hours of ventilation daily. They observed that he could only breathe without the ventilator for a maximum of 90 minutes at a time. Recognising the potential impact on Salem's quality of life, the medical team proposed Phrenic Nerve Pacing (PNP) as an alternative to a tracheostomy.
PNP is a surgical/medical procedure where a breathing pacemaker is surgically implanted on to the phrenic nerves. These nerves play a vital role in transmitting signals from the brain to the diaphragm, the main breathing muscle under the lungs. In children with ROHHAD syndrome, these signals are not sent correctly from the brain, resulting in insufficient breathing. PNP involves electrically stimulating the phrenic nerves to trigger diaphragm contraction and stimulate breathing. PNP requires a small operation to attach wires to the phrenic nerves on both sides of the chest. These wires then transmit to a small pacing box which the child can carry in a backpack. The pacing box can be adjusted by the medical team to alter the rate and power of stimulation that is provided to the diaphragm.
In some cases, PNP can be used to avoid mechanical ventilation completely. However, due to the severity of Salem's hypoventilation, the medical team recommended that PNP could aid his breathing during the day, while at night, he should use a standard ventilator with a mask. This approach would allow him to avoid a tracheostomy and have a much better quality of life.
Explaining the reasoning behind their proposed strategy, Dr Martin Samuels said "conventional mechanical ventilation typically necessitates invasive techniques like tracheostomy or the application of a face mask, both of which involve bulky equipment and restrict daytime mobility."
Phrenic Nerve Pacing (PNP) presents a discreet alternative by stimulating the diaphragm, enabling natural breathing without the requirement for cumbersome apparatus. Utilising a compact and lightweight external pacing box allows Salem to significantly enhance his mobility during the day, providing a more comfortable and inconspicuous solution for his respiratory challenges.
Dr Martin Samuels
The next step was to assess Salem for the surgical procedure. For this the team called in Mr Stefano Giuliani, who is an experienced paediatric surgeon at GOSH, well-versed in the surgical implantation of PNP from his training at Los Angeles Children's Hospital. Mr Giuliani collaborated with the team to engage in thorough discussions with Salem's family. They provided comprehensive explanations regarding every aspect of PNP, ranging from the surgical procedure to its long-term implications. After reviewing all the information and addressing numerous queries, Salem's family expressed a firm decision to proceed with the surgery.
The surgical team took the time to explain every step to us. We felt a sense of comfort knowing that Salem was in capable hands.
Salem’s Grandmother
Before the surgery, the GOSH team meticulously reviewed all the steps involved, prioritising safety at every stage of the process. Additionally, they communicated with local doctors in Qatar, ensuring their agreement with the decision to initiate PNP for Salem and confirming their willingness to manage the system long-term with GOSH's support. The Qatari doctors expressed eagerness to proceed with the plan.
Additionally, Salem needed to have a full medical evaluation for other features of ROHHAD as it is a very rare and complex condition that can impact upon multiple body systems and can make surgery hazardous. Salem underwent thorough reviews with experts in cardiology, endocrinology, gastroenterology, and oncology. These specialists, experienced in treating children with ROHHAD, were familiar with potential complications. Fortunately, all the investigations were normal, and surgery was able to proceed.
ROHHAD is a very unusual condition, and it is essential that children with this diagnosis are reviewed by multiple specialists who have experience in dealing with it. We are very fortunate at GOSH to have all the expertise on one site. In addition, we were able to reassure our colleagues in Qatar that we would provide long term support, not just for the PNP system but also for any other medical complications that Salem could develop in future.
Dr Paul Aurora
Salem's PNP surgery involved the implantation of special electrodes connected to the phrenic nerves on either side of his chest. The electrodes would stimulate his diaphragm, helping him breathe more effectively during the daytime. The surgery was performed with an innovative minimally invasive technique (thoracoscopy) which favours a quick recovery with less post-operative pain compared to traditional open surgery.
Salem’s operation to implant the phrenic nerve pacing has been a true success and the first of this kind in the UK in a child. The procedure was the effort of an international collaboration with Dr Cathy Shin, a paediatric surgeon from Los Angeles, who is a world expert in this minimally invasive technique.
Mr Stefano Giuliani

Following the surgery, Salem stayed at GOSH for a recovery period. Once the postoperative swelling had subsided, the medical team started using the PNP. Throughout this period, thorough assessments and regular adjustments were made as needed to ensure the appropriate level of support, guaranteeing Salem's adequate and comfortable breathing. The process took a few weeks, but the end result was excellent. Salem was able to breathe on his own with the support of the PNP system and without the need for his ventilator during the daytime. The system worked well when he was resting, but also during activities such as walking, running, and playing. He was even tested inside a simulated flight cabin where the oxygen levels in the air are lower.
Salem benefited from monitoring by the sleep and long-term ventilation teams which included sleep physiologists, nurse specialists, and medical consultants. They closely supervised and reviewed Salem's sleep studies as part of his clinical management plan, ensuring prompt addressing of any issues. Daytime recordings, guided by sleep physiologists, helped adjust PNP settings under sleep consultants' supervision.
“This tailored approach in his continual monitoring was crucial in Salem's recovery journey, ensuring the safety and effectiveness of his treatment (PNP in the daytime and non-invasive respiratory support at night), especially since he relies on PNP and non-invasive ventilation to sustain his breathing” highlighted Dr. Elaine Chan.
At GOSH, we conduct sleep studies with live titration for ventilation and PNP, enabling customised settings for patients like Salem who depend on technology for respiratory support.
Dr. Elaine Chan
“During our challenging time here, I felt that the nurses, doctors, and all the staff were like family to us. They provided the reassurance we needed and explained everything we needed to know along the way” explained Salem’s Grandmother.
During this period the team also trained the family in how to use and check that the system, was working correctly. This training went very well, and Salem was able to be discharged and returned home to Qatar. For the first time in a year, he was now able to be looked after at home.
The medical team guided us through every aspect of Salem's adjustment to the pacing device. Their dedication made us feel assured, knowing Salem was under capable and caring hands. We were actively involved in the process, and the hospital's support in helping us understand how to operate the external pacing box was invaluable.
Salem’s Grandmother

Since Salem’s return to Qatar, Dr Aurora has stayed in touch with the local team to check on his progress which has been very positive.
The surgery went very well, without any complications. Just as importantly, the system functioned exactly as we hoped and predicted it would. It was completely effective in stimulating Salem’s breathing when he was awake, meaning that he had no need to use a ventilator machine. This has transformed Salem’s quality of life. He is able to spend his whole day without a ventilator, just carrying his pacing box in a backpack. With this he can do all activities with his family and attend school. He is even able to remove the box for a short period so that he can go swimming. This is his favourite hobby, so he is delighted by this.
Dr Paul Aurora
“Seeing Salem embrace normal activities; is truly heart-warming it brings much joy to our family” said Salem’s Grandmother.
Salem's family is scheduled for a follow-up appointment at GOSH six months post-surgery to assess his breathing and the functionality of the PNP device. Regular monitoring and check-ups back in Salem’s hometown are also planned to ensure Salem's ongoing well-being.
Salem’s treatment was led by Dr Paul Aurora, Dr Martin Samuels, Mr Stefano Giuliani, and Dr Elaine Chan. The success of this treatment would not have been achievable without the unwavering support of an extensive team, including specialists in cardiology, endocrinology, oncology, radiology, anaesthesia, operating theatre staff, intensive care, respiratory physiology, surgical and respiratory nursing, laboratory personnel, porters, and other support staff. Their combined expertise and skills facilitated a thorough evaluation of Salem's medical needs, ensuring the success of this innovative treatment.
Children with highly complex and life-threatening conditions can be very difficult to care for. Local doctors may not have seen similar children before and may be unsure as to which investigations or treatment are necessary. This is when a referral to a highly specialised centre like Great Ormond Street Hospital can be so helpful. We have so many highly experienced specialists here who have seen rare cases before and will work carefully together to solve the most complicated problems. Salem’s complicated situation and his highly successful treatment is a perfect example of how well this hospital can work.
Dr Paul Aurora
Salem's case exemplifies the collaborative and comprehensive approach to care at GOSH. The successful implementation of phrenic nerve pacing not only addressed Salem's respiratory challenges but also allowed him to return to a more normal and active life. This case highlights the importance of tailored solutions for complex medical conditions and the positive impact of specialised care provided by GOSH.
Salem is one of the first two PNP cases implemented at GOSH, currently only available through self-funded care while the National Institute for Health Care Excellence (NICE) is currently evaluating the evidence for PNP to determine its potential availability in the UK.


