First UK trial of Deep Brain Stimulation for children with epilepsy begins
A GOSH patient who was the first patient to take part in a UK clinical trial to use deep brain stimulation (DBS) to treat epilepsy has seen daytime seizures reduce by 80%.
The rechargeable device is mounted onto the skull and is attached to electrodes deep in the brain to reduce seizure activity. This is the first UK clinical trial measuring this type of treatment for children with epilepsy. The CADET pilot (Children’s Adaptive Deep brain stimulation for Epilepsy Trial) will now recruit three additional patients with Lennox-Gastaut syndrome, which is funded by the Royal Academy of Engineering, before 22 patients take part in the full trial, which is being funded by GOSH Charity and LifeArc. The study is sponsored by University College London.
Every single day we see the life-threatening and life-limiting impacts of uncontrollable epilepsy. It can make school, hobbies or even just watching a favourite TV show utterly impossible... Deep brain stimulation brings us closer than ever before to stopping epileptic seizures for patients who have very limited effective treatment options. We are excited to build the evidence base to demonstrate the ability of deep brain stimulation to treat paediatric epilepsy and hope in years to come it will be a standard treatment we can offer.
Martin Tisdall, Consultant Paediatric Neurosurgeon at GOSH and Honorary Associate Professor at UCL
The CADET Pilot and Trial
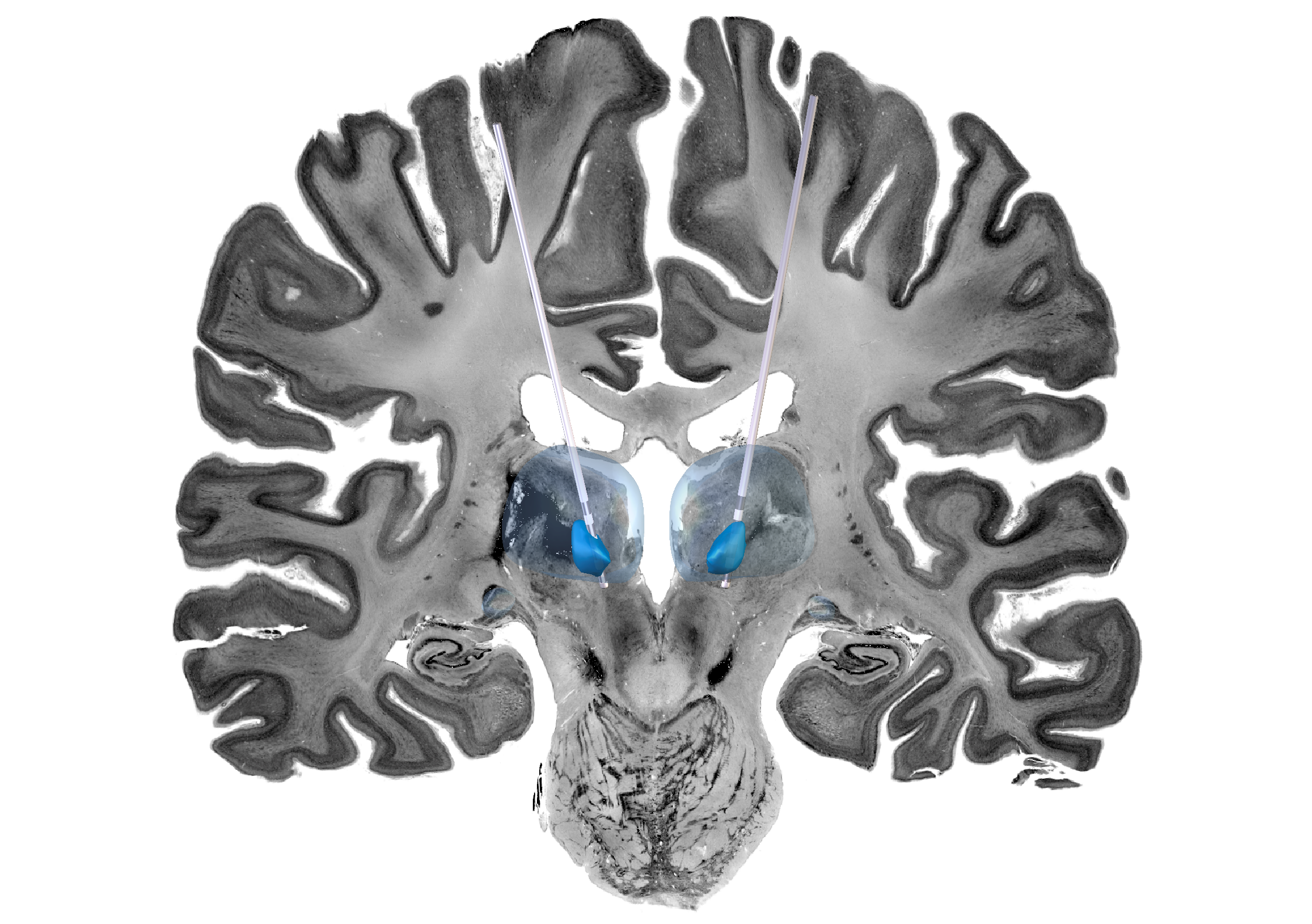
Deep Brain Stimulation (DBS) is a treatment involving surgery to insert a small device which stimulates specific parts of the brain.
Unlike other DBS devices which are mounted on the chest with wires running up the neck to the brain, this device is mounted on the skull meaning the leads are less likely to break or erode as the child grows.
This device is also rechargeable through wearable headphones, which can be used while watching a video or interacting with a tablet. This also means it does not require surgery to replace it every three to five years.
The device targets the thalamus, which is a hub for electrical signals in the brain. It is hoped that the device will block electrical pathways and consequently stop seizures from spreading. The device also has settings for optimisation towards seizure patterns, which although not utilised in this trial, could be used in the future for patients with LGS.
Our mission is to design pioneering research systems for exploring the treatment of intractable health conditions such as paediatric epilepsy. This is the first patient in the world to receive this device and we are extremely pleased that it has had such a positive benefit for him and his family.
Professor Tim Denison, University of Oxford and Royal Academy of Engineering Chair in Emerging Technologies
The CADET Pilot is funded by the Royal Academy of Engineering and sponsored by University College London. It is a collaboration between GOSH, UCL, King’s College London, the University of Oxford and a UK-based company: Amber Therapeutics.
The second phase of the trial will be jointly funded through GOSH Charity and LifeArc’s Translational Research Accelerator Grants.


