'Mini eyes’ help researchers understand blindness in rare condition
Researchers at UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) have grown ‘mini eyes’ in the lab which will help researchers understand how blindness develops in the rare genetic condition Usher syndrome.
What is Usher syndrome?
Usher syndrome is a rare inherited condition that affects hearing and vision, and often balance. It is the most common genetic cause of combined deafness and blindness, affecting approximately three to ten in 100,000 people worldwide.
There are three types of Usher syndrome. Children with Type 1 Usher syndrome, the most severe form, are often born profoundly deaf, while their sight slowly deteriorates until they are blind by adulthood.
Although cochlear implants can help with hearing loss, there are currently no treatments for retinitis pigmentosa, which is the cause of vision loss in Usher syndrome.
New ways to study vision loss
Previously it had been difficult to study vision loss in Usher syndrome because animal cells couldn’t mimic the same sort of sight loss as that seen in the condition.
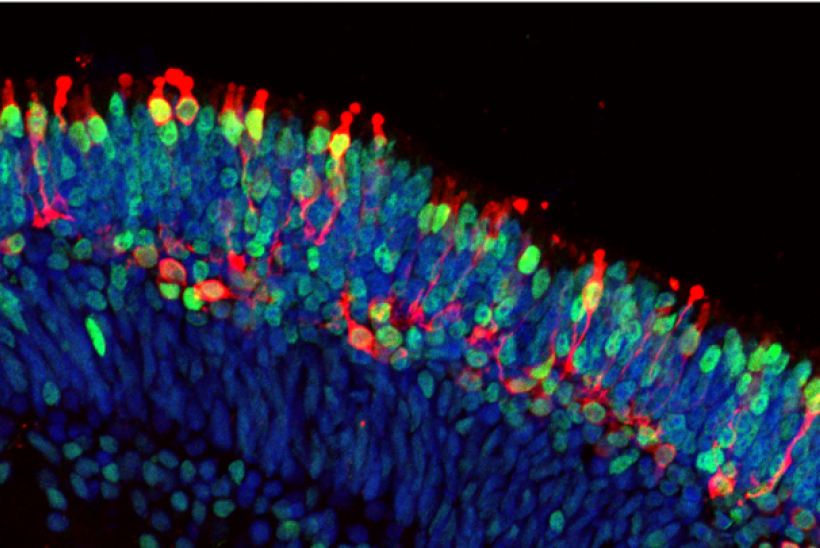
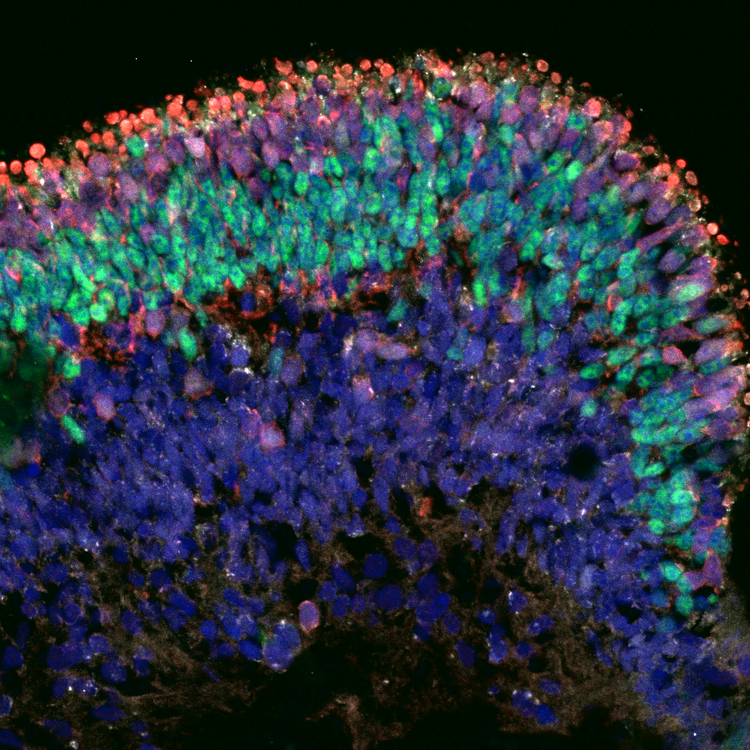
Now, researchers at UCL GOS ICH have grown 3D ‘mini eyes’, called organoids, that enable them to study the development of blindness. In a healthy eye, rod cells - the cells which detect light - are arranged in the back of the eye in an important region responsible for processing images called the retina. In this research, published in Stem Cell Reports, the team found that they could get rod cells to organise themselves into layers that mimic their organisation in the retina, producing a ‘mini eye’.
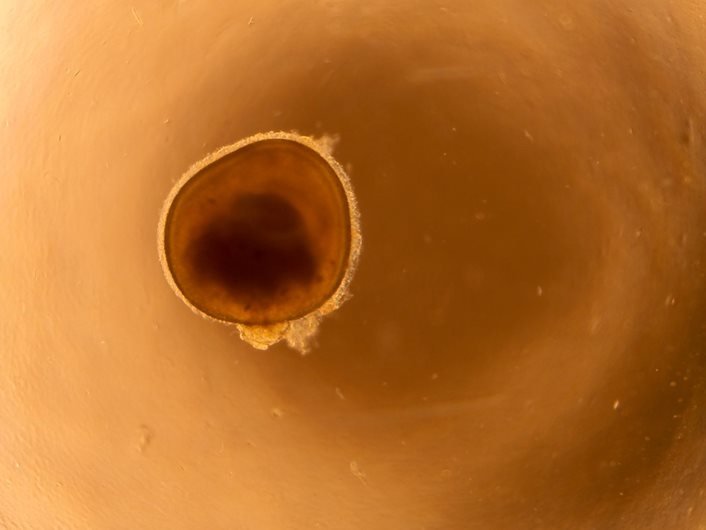
The ‘mini eyes’ were grown from stem cells generated from skin samples donated by patients at Great Ormond Street Hospital for Children (GOSH). As the ‘mini eyes’ are grown from cells donated by patients with and without the genetic ‘fault’ that causes Usher syndrome, the team are able to compare healthy cells and those that will lead to blindness.
Understanding these differences could provide clues to changes that happen in the eye before a child’s vision begins to deteriorate. In turn, this could provide clues to the best targets for early treatment, which would be crucial to providing the best outcome.
New findings
The ‘mini eyes’ are an important step forward in research, allowing the team to study light-sensing cells from the human eye in more detail than ever before.
For example, using powerful single cell RNA-sequencing, it is the first-time researchers have been able to view the tiny molecular changes in rod cells before they die.
The team also discovered that Müller cells, responsible for metabolic and structural support of the retina, are also involved in Usher syndrome. They found that cells from people with Usher syndrome abnormally have genes turned on for stress responses and protein breakdown. Reversing these could be the key to preventing how the disease progresses and worsens.
It’s difficult to study the inaccessible tiny nerve cells of the patient’s retina as they are so intricately connected and delicately positioned at the back of the eye. By using a small biopsy of skin, we now have the technology to reprogramme the cells into stem cells and then create lab-grown retina with the same DNA, and therefore same genetic conditions, as our patients.
Doctor Yeh Chwan Leong, Research Associate at UCL GOS ICH and first author on the study
Supporting future research
The ‘mini eye’ model for eye diseases is not only useful for studying Usher syndrome, but could also help teams understand other inherited conditions in which there is the death of rod cells in the eye, such as forms of retinitis pigmentosa without deafness.
The technology used to grow faithful models of disease from human skin cells can also be used for several other diseases - this is an area of expertise at the Zayed Centre for Research into Rare Disease in Children at UCL GOS ICH.
Continuing this pioneering work, researchers hope to create ‘mini eyes’ from more patient samples, and use them to help identify treatments, for example by testing different drugs. In the future, it may be possible to edit a patient’s DNA in specific cells in their eyes to avoid blindness.
We are very grateful to patients and families who donate these samples to research so that, together, we can further our understanding of genetic eye conditions, like Usher syndrome.
Although a while off, we hope that these models can help us to one day develop treatments that could save the sight of children and young people with Usher syndrome.
Professor Jane Sowden, Professor of Developmental Biology & Genetics at UCL, and senior author on the study
This research was funded by National Institute for Health and Care Research Great Ormond Street Hospital Biomedical Research Centre (NIHR GOSH BRC), Medical Research Council, GOSH Children's Charity and Newlife the Charity for Disabled Children.
All research at Great Ormond Street Hospital is underpinned by support from the NIHR GOSH BRC.